Article Notes
- Powered air-purifying respirator (PAPR) with coverall may be more protective than N95 masks and gown (RR 0.27), but create unique donning challenges.
- Long-gowns may be better than a coverall, but are also more difficult to doff. Gowns are better than aprons. Better sealing, fitting, and one-piece removal at gown-glove interfaces and closer fit around the neck may reduce exposure.
- Double-gloving may reduce exposure.
- Better training, computer simulation, video lectures, following CDC protocols, and spoken instruction may improve donning and doffing compliance.
- Laryngeal activity - talking, coughing, sneezing.
- High velocity gas flow - eg. high-flow oxygen
- Cyclical opening & closing of terminal airways.
- Despite this history we remain unprepared for a pandemic.
- From an ICU perspective, conservative models predict >170% ICU resource utilisation due to a pandemic. They note that most health systems would struggle with even this optimistic surge.
- SARS experience in Canada, despite only 251 cases, critically stretched hospital and ICU resources.
- Pandemic surveillance.
- Prepare health-system scalability to manage surge: equipment, physical space, human resources, and system (eg. stepped triage plans).
- Prepare for mass vaccine production.
- Better coordinate and integrate communications.
- Streamlined research and ethics proposals for rapid initiation.
- Virtue ethics – behaving in the way we think is right; embodying courage.
- Utilitarianism – behaving so as to maximise the best outcomes for the greater number of people.
- Deontology – obeying the rules; following a duty to moral law.
- Principlism – balances beneficence, nonmaleficence, autonomy and justice.
- It is clinical outcomes that primarily matter, and;
- Simulation is uniquely positioned to address improvements in the many domains of teamwork.
This is the second update to Verbeek et al.'s 2016 Cochrane Review of personal protective equipment (PPE) for preventing infections in healthcare workers (HCW). The prior update was in July 2019.
What's worth knowing?
Overall most studies of PPE efficacy are of low quality and offer a low certainty of conclusions. Caveat emptor...
In this review, Wilson, Norton, Young & Collins challenge the overly-simplistic view that SARS-CoV-2 transmission risk can be easily divided between droplet-contact and aerosol precautions.
Why is this important?
Many national societies have policies on Personal Protective Equipment (PPE) guided by classification of COVID exposure into aerosol-generation procedures (AGP) or other exposures. Although founded in some evidence, there are questions as to whether PPE shortage and availability also drives these recommendations. Widespread concern over healthcare worker (HCW) infection is understandable, given that during SARS 20% of infections were among HCWs.
Understanding the science behind respiratory particle generation and transmission helps to inform our understanding of how best to use limited PPE.
On the science of respiratory shedding
Aerosol generation is important because virus inhalation and deposition in small distal airways may be associated with greater infection risk and disease severity. Wilson et al. describe three mechanisms of aerosol generation:
Notably, the clinically features of COVID itself make all three high-risk mechanisms more likely. Additionally various studies show that even talking and tidal volume breathing produce large numbers and size ranges of respiratory droplets.
Exposure relative risk is primarily about proximity and exposure duration
Further, considering retrospective data form SARS HCW infections involving various procedures (eg. intubation, HCW infection RR 4.2; oxygen mask manipulation RR 9; urinary catheterisation RR 5), Wilson et al. propose that healthcare work risk can be considered:
infection risk ∝ 𝑏 × 𝑣 × 𝑡 / 𝑒
Where: 𝑏 = breathing zone particle viable virion aerosol concentration, 𝑣 = minute volume of healthcare worker, 𝑡 = time exposed , 𝑒 = mask efficiency
And on intubation:
"...[other] healthcare workers should stand over 2 m away and out of the direct exhalation plume. During a rapid sequence intubation muscle relaxation should be protective as coughing will be prevented and high airway gas flow and expiratory output will terminate. When expiratory flow is ended ... aerosol particles should start settling in the airways. The forces generated in gentle laryngoscopy are unlikely to cause aerosol formation."
"...[there is] limited evidence to suggest AGPs cause an increase in airborne healthcare worker transmission as this has not been studied. The few studies to sample pathogenic airborne particles in relation to procedures show no increase with the majority of AGPs."
Bear in mind...
Much of the evidence guiding our understanding of SARS-CoV-2 transmission is founded on understanding and research focusing on the 2003 SARS pandemic (SARS-CoV-1) and influenza research. Although sharing similarities, "...each has its own infective inoculum and aerosol characteristics."
What's the bottom-line?
Transmission of SARS-CoV-2 should be conceptualised as a spectrum of risk where time exposed may be the dominant factor and droplet-airborne spread is a complex continuum of varying probability of infection. Many 'non-AGP' events could in fact be higher risk than those traditionally considered AGP, such as intubation.
What is this?
Kain & Fowler's prescient review from October 2019 sets out how intensive care units should prepare and respond to the next pandemic, both practically at a hospital level and at a wider health-system. Although the focus was on an influenza pandemic, the advice is readily applicable to the SARS-COV-2 pandemic.
Background
They note that not only have we seen regular influenza outbreaks in addition to other viral pandemics, that due to increased urbanisation, population density, global travel and living proximity to animals, there is rapidly increasing global risk of a viral pandemic.
"When considering preparation for the next pandemic, it is not a matter of if it will occur, but rather a matter of when." – Kain & Fowler
They provide an overview of historical influenza pandemics over the last century, most recently with the 2009 H1N1 swine-flu pandemic, killing 300,000 people.
What preparation do they recommend?
Kain and Fowler suggest global focus on:
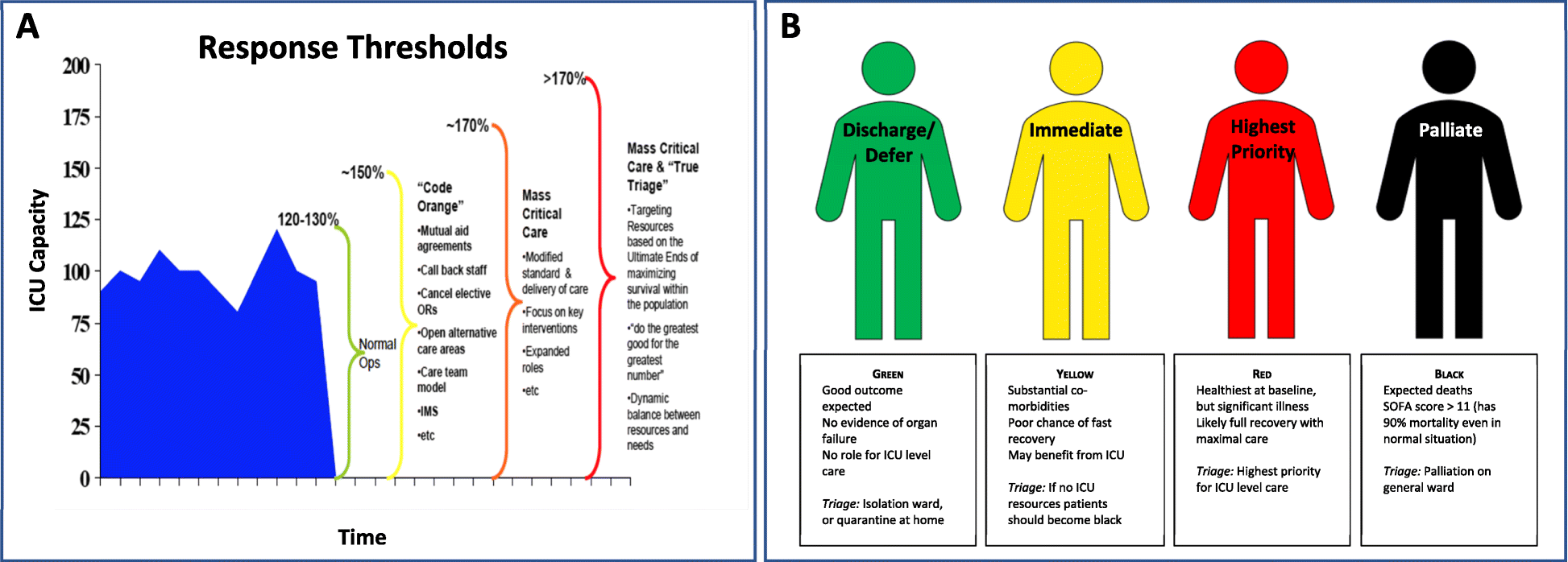
They highlight the importance of intensivists being involved in strategic planning, so as to coordinate ICU responses for "...triage, clinical care, and infection control." – noting that during SARS 20% of infections were in healthcare workers, and hospitals themselves became important sources of transmission.
Final word...
The IHR Committee's review following the 2009 H1N1 pandemic is now only too obvious:
“...the world is ill-prepared to respond to a severe influenza pandemic or to any similarly global, sustained, and threatening public-health emergency.” – International Health Regulations Committee (2011)
An exploration of the ethics, challenges and practical reality of treating family members. Hutchison & McConnell deploy models of virtue, utilitarianism, deontology and principlism in an accessible and applied way.
They cautiously challenge the blanket prohibitions of many professional bodies against treating family members.
Well worth reading.
“Only by constantly questioning whether they are the correct person to deliver care can they hope to do right by both their relative and themselves.”
Why is this important?
Although we have moved beyond routinely using high tidal volumes in favour of ’protective ventilation strategies’ the specifics of what is protective and what improves outcomes is controversial. Previous trials have struggled to demonstrate post-operative respiratory benefits from protective strategies.
What did they do?
In this small randomised controlled trial, Généreux et al. investigated whether intraoperative PEEP (7 cmH2O) and recruitment manoeuvres (RM) q30min would reduce atelectasis post-extubation. Using ultrasound to measure intraoperative and post-operative atelectasis gives their study greater flexibility than other studies using CT scanning, generally considered the gold standard for atelectasis measurement.
And they found...
Among 34-85 yo women undergoing open gynae-oncology surgery >2h duration, there was no post-extubation difference in atelectasis whether receiving PEEP/RM or zero PEEP.
Not so fast
There was however less intraoperative atelectasis among the protective ventilation group, supporting the common use of PEEP and RM to improve oxygenation during surgery. Additionally, they specifically excluded morbidly obese women (BMI > 40 kg/m2), an increasingly common demographic at risk of ventilation challenges.
Nonetheless this study adds to the evidence that current protective ventilation strategies do not actually reduce post-operative respiratory complications.
Be smart
One interesting observation was the large amount of inter-patient variability, the researchers noting:
“...this heterogeneity highlights the need to dynamically monitor lung aeration changes and personalise our delivery of mechanical ventilation in the perioperative setting.”
As with many perioperative interventions, the benefits may in fact lie in the personalisation of our care for each individual patient.
Why is this important?
Most simulation research focuses on skills and knowledge (the easiest factors to measure), even though:
Brazil et al. applied a relational coordination (RC) framework to understand teamwork-aspects of simulation research, particularly as these impact wider institutional and healthcare system performance.
“The RC framework — shared knowledge, shared goals and mutual respect in the context of communication that is timely, accurate, frequent and problem-solving based — can provide a common language for simulation educators to design and debrief simulation exercises that aim to have a translational impact” (Brazil et al. 2019)
What did they do?
The researchers undertook a narrative survey of staff involved in early major trauma care at a university teaching hospital. Over half of the respondents had participated in the institution’s existing in situ trauma simulation program.
Survey responses were analysed using the RC framework, and found to be consistent with each RC domain. Most notably trauma simulation acted as an enabler of mutual respect and improved communication, along with enhancing the understanding of team roles and prioritising problem-solving focused communication.
The take-home
The impact of simulation needs to be understood in the context of the greater goal – healthcare system improvement – and that this occurs with pre-existing organisational cultures and relationships. Simulation outcomes goals are not exclusive to small teams or individual performance.
The various domains within the relational coordination framework provide an easy to use guide for understanding, communicating and deploying simulation benefits, drawing a path from the ‘here’ to the ‘there’ of improved outcomes.
“Simulation should be considered as a tool to build and strengthen relationships between practitioners across traditional boundaries.”