Article Notes
- Despite this history we remain unprepared for a pandemic.
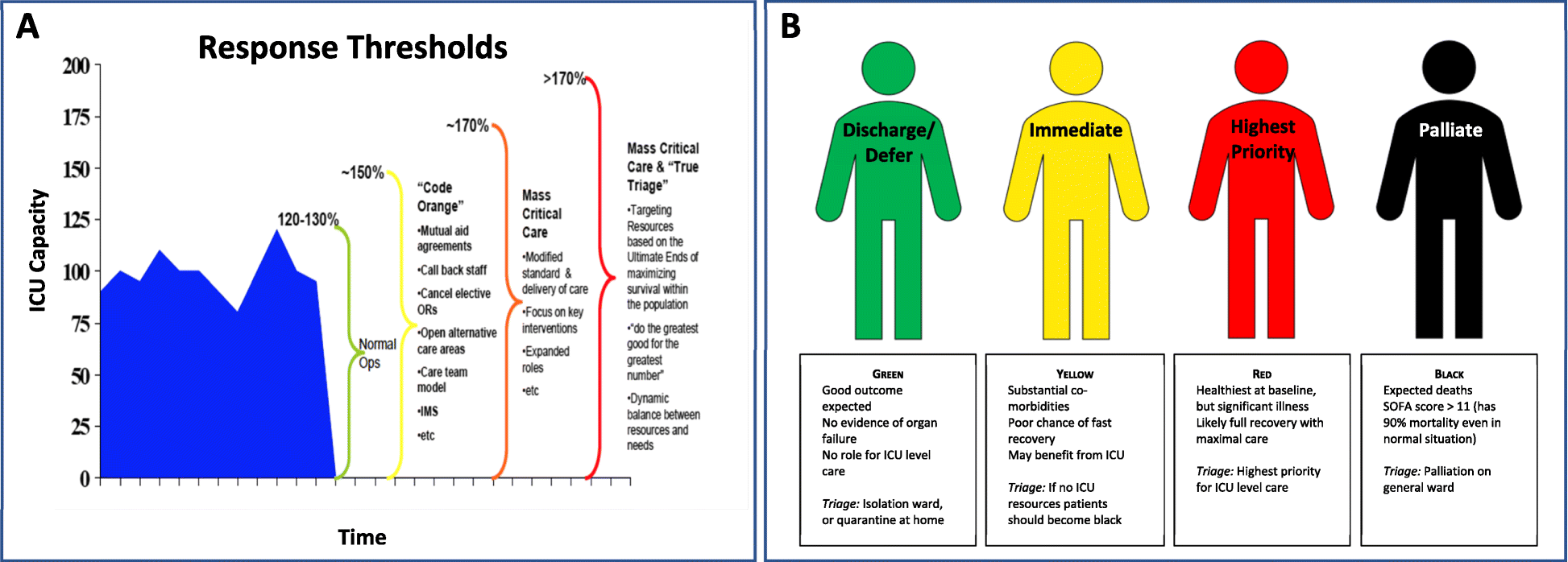
- From an ICU perspective, conservative models predict >170% ICU resource utilisation due to a pandemic. They note that most health systems would struggle with even this optimistic surge.
- SARS experience in Canada, despite only 251 cases, critically stretched hospital and ICU resources.
- Pandemic surveillance.
- Prepare health-system scalability to manage surge: equipment, physical space, human resources, and system (eg. stepped triage plans).
- Prepare for mass vaccine production.
- Better coordinate and integrate communications.
- Streamlined research and ethics proposals for rapid initiation.
- Virtue ethics – behaving in the way we think is right; embodying courage.
- Utilitarianism – behaving so as to maximise the best outcomes for the greater number of people.
- Deontology – obeying the rules; following a duty to moral law.
- Principlism – balances beneficence, nonmaleficence, autonomy and justice.
What is this?
Kain & Fowler's prescient review from October 2019 sets out how intensive care units should prepare and respond to the next pandemic, both practically at a hospital level and at a wider health-system. Although the focus was on an influenza pandemic, the advice is readily applicable to the SARS-COV-2 pandemic.
Background
They note that not only have we seen regular influenza outbreaks in addition to other viral pandemics, that due to increased urbanisation, population density, global travel and living proximity to animals, there is rapidly increasing global risk of a viral pandemic.
"When considering preparation for the next pandemic, it is not a matter of if it will occur, but rather a matter of when." – Kain & Fowler
They provide an overview of historical influenza pandemics over the last century, most recently with the 2009 H1N1 swine-flu pandemic, killing 300,000 people.
What preparation do they recommend?
Kain and Fowler suggest global focus on:
They highlight the importance of intensivists being involved in strategic planning, so as to coordinate ICU responses for "...triage, clinical care, and infection control." – noting that during SARS 20% of infections were in healthcare workers, and hospitals themselves became important sources of transmission.
Final word...
The IHR Committee's review following the 2009 H1N1 pandemic is now only too obvious:
“...the world is ill-prepared to respond to a severe influenza pandemic or to any similarly global, sustained, and threatening public-health emergency.” – International Health Regulations Committee (2011)
An exploration of the ethics, challenges and practical reality of treating family members. Hutchison & McConnell deploy models of virtue, utilitarianism, deontology and principlism in an accessible and applied way.
They cautiously challenge the blanket prohibitions of many professional bodies against treating family members.
Well worth reading.
“Only by constantly questioning whether they are the correct person to deliver care can they hope to do right by both their relative and themselves.”